How MAP Delivers ROI
58% Reduction in total post-acute PMPM costs, including:
Reduction in treatment readmissions
Reduction in downstream ER visits
Reduction in non-routine doctor visits
How We Could Save You $20 Million:

On average, let's assume a 30 day stay at an inpation addiction treatment facility costs:

$20,000 (in network)*
$40,000 (out of network)*

If you stay engaged with 1,000 members post-acute this can prevent them from going out of network and you would save:

~$20,000,000
Models for Improving Outcomes in Substance Use Disorder
MAP identifies highest risk members and MAP Care Solutions team provides post-acute engagement services. Provider and Payer receive outcomes reporting
Identify the quality metrics that drive outcomes and incentivize providers to shift toward a shared risk model. Includes provider and member engagement plans
MAP customizes a comprehensive solution based on our initial assessment and a comprehensive process for your network PCP’s to integrate with our solutions platform
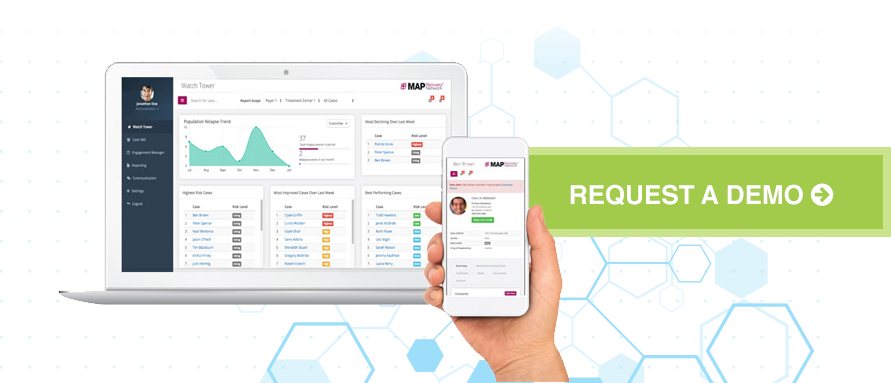
Where Does The Data Come From?
Members
Member reported data derived from post-aucte engagements via telehealth
Consents
Passive interview and validation of member inputs

Devices & Apps
Remote Breathalyzer, Med Adherence and Dispensation, Anxiety Monitors, Pharmacogenetics, Self-management apps

EMR/EHR Integrations
MAP's interoperable platform integrates with existing clinical workflows where appropriate to eliminate redundancy

Administrative Platforms
Eligibility for enrollment and cost data for ROI analysis, and census data for hospitalization