Solutions for Payers
Improve care, improve outcomes and reduce costs.
Our solutions enable the discovery of insights through proactive care management, intuitive cost/performance reporting, provider performance management and holistic behavioral health population management.
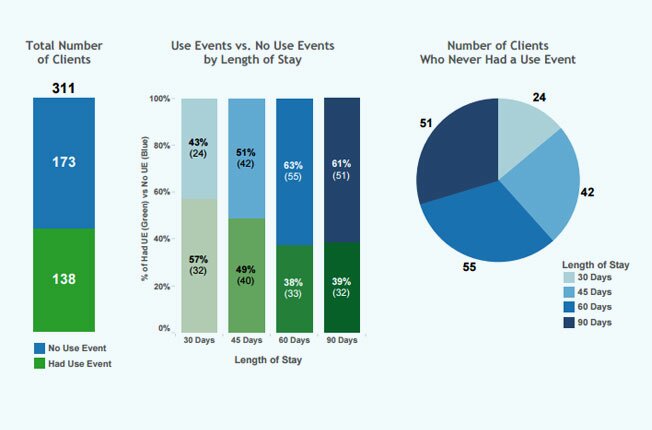
Reduce Costs
Improving the patient and provider experience through reliable and timely data reduces healthcare costs across the entire healthcare landscape.
Measure Performance
Performance measurement is synthesized into an intuitive dashboard that delivers key data that allows providers to assess patient risk, observe trends, and manage staff workloads to improve performance.
Increase Engagement & Prevent Loss
It’s vital that payers and providers keep members enrolled and reduce costs and quality loss of the member going out of network. The cost of treatment in Behavioral Health and SUD can be dramatically reduced by keeping patients in-network.
Expand Access to Care
MAP's Telehealth Platform improves a client's chances of achieving and maintaining long-term recovery and enhances your ability to care coordinate through primary care integration.
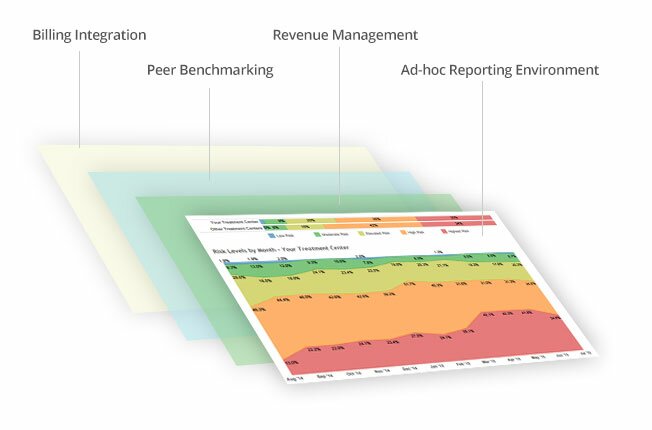
How MAP Delivers Value
MAP’s platform captures a unique and expansive data set that delivers actionable insights to improve clinical and financial outcomes for behavioral health and addiction treatment. At a high level, MAP works with payers to deliver and optimize: